How to Treat Scalp Infections That Lead to Hair Loss
- Last Updated on

Image: healthline.com
Scalp infections are a common but often misunderstood cause of hair loss. They can result from fungal, bacterial, or inflammatory skin conditions that disrupt the natural hair growth cycle, leading to temporary or permanent thinning. Early intervention is crucial for minimizing damage and promoting regrowth. This article provides a comprehensive overview of evidence-based approaches for managing scalp infections, including what you need, what to do, and how often.
Articles Contains
- Solutions For Scalp Infection: Types and Treatments
- Final Words
- Key Takeaways
- Frequently Asked Questions
- References
Solutions for Scalp Infections: Types and Treatments
1. Fungal Infections (Tinea Capitis)
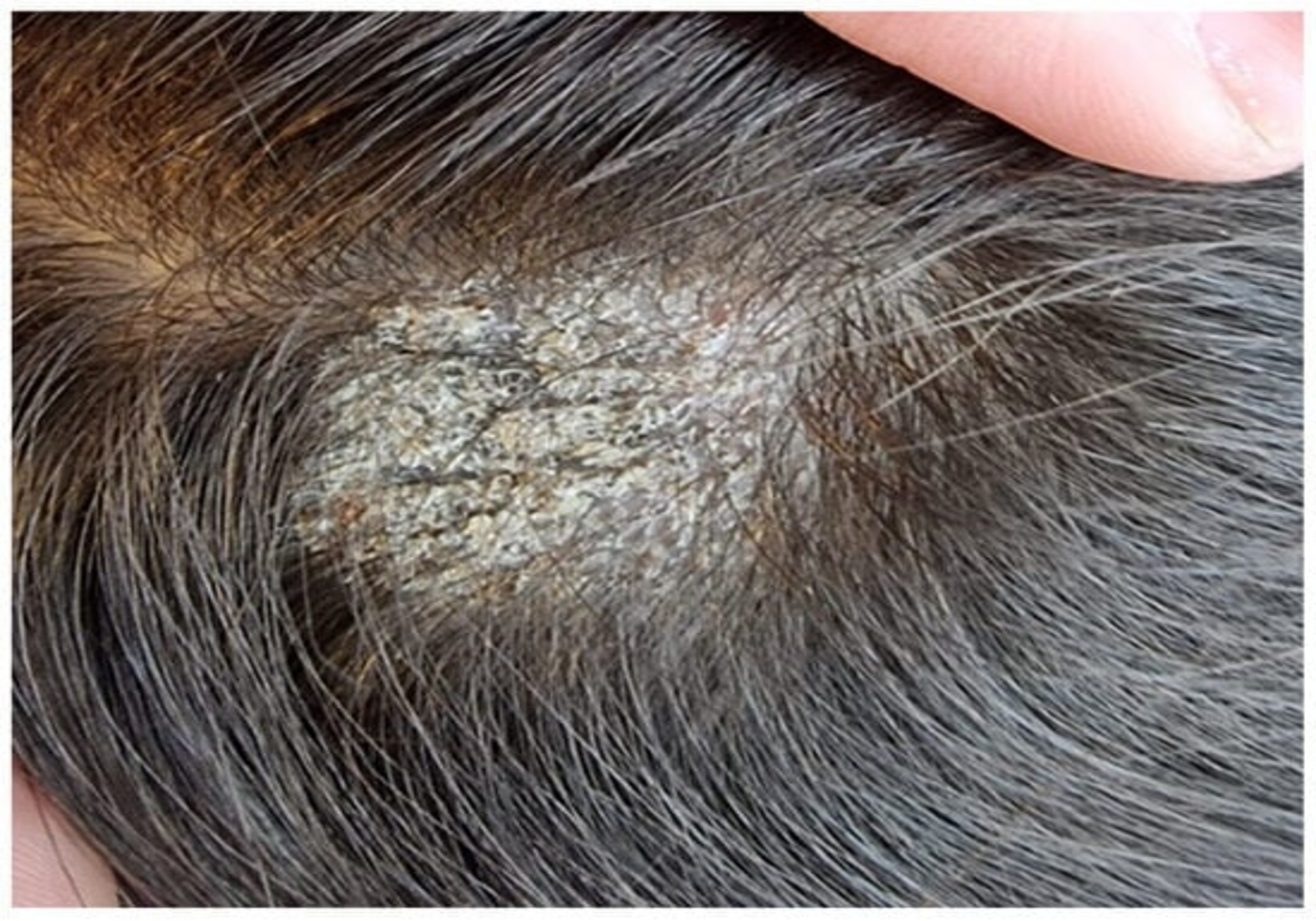
Image: mdpi.com
What You Need
- Oral antifungal medications: Griseofulvin, terbinafine, or itraconazole (5) are the most effective treatments for tinea capitis, as they penetrate the hair follicle to eliminate the fungus.
- Antifungal shampoos: Products containing ketoconazole or selenium sulfide can help reduce fungal shedding, decreasing the risk of spreading the infection but are insufficient as standalone treatments (2).
What to Do
- Take oral antifungal medications as prescribed by a healthcare professional. These are the cornerstone of treatment, as topical agents cannot adequately reach infected hair shafts.
- Wash the scalp with an antifungal shampoo twice weekly to supplement systemic therapy and reduce surface fungal load.
How Often
- Oral antifungals: Daily for 4–8 weeks or until the infection is resolved.
- Antifungal shampoos: Use 2–3 times per week during treatment and as directed by a healthcare provider.
Additional Tips
- Disinfect personal items like combs, brushes, and pillowcases regularly to prevent reinfection (Reference 3).
- Avoid sharing hair tools or accessories, especially in group settings, to reduce the risk of fungal transmission.
2. Bacterial Infections (Folliculitis and Folliculitis Decalvans)
Bacterial infections, such as folliculitis or its severe variant folliculitis decalvans, occur when bacteria like Staphylococcus aureus infiltrate hair follicles, leading to inflammation, pustules, and sometimes scarring. Folliculitis decalvans is a chronic condition that can cause irreversible hair loss if untreated. Prompt diagnosis and aggressive treatment are vital (4).

Image: wikipedia.org
What You Need
- Oral antibiotics: Common options include doxycycline, clindamycin, or a combination of clindamycin and rifampicin, particularly for resistant cases.
- Topical antibacterial treatments: Mupirocin ointment or chlorhexidine washes are effective for localized infections and preventing bacterial spread.
What to Do
- A healthcare provider may prescribe oral antibiotics for moderate to severe infections. These reduce bacterial load and inflammation, allowing follicles to heal.
- Apply mupirocin ointment to affected areas as directed. Use antibacterial washes for mild cases or as an adjunct to systemic therapy.
How Often
- Oral antibiotics: Taken daily for 2–4 weeks, depending on the severity of the infection.
- Topical treatments: Use twice daily or as prescribed by your healthcare provider.
Additional Tips
- Refrain from scratching or picking at pustules, as this can worsen infection and spread bacteria (5).
- Maintain good scalp hygiene by washing your hair regularly with a gentle, medicated shampoo.
3. Seborrheic Dermatitis
Seborrheic dermatitis is a common inflammatory condition that causes red, scaly patches on the scalp and may contribute to temporary hair loss. While the exact cause is unknown, it is often linked to an overgrowth of Malassezia yeast and increased oil production. Chronic cases can weaken hair follicles and exacerbate shedding (6).

Image: ferraraderm.com
What You Need
- Medicated shampoos: Products containing zinc pyrithione, ketoconazole, or salicylic acid are effective for reducing inflammation and yeast overgrowth.
- Topical corticosteroids: Mild corticosteroid creams or lotions can help control flare-ups and alleviate itching.
- Moisturizers: Hypoallergenic and non-comedogenic scalp moisturizers soothe dryness and scaling.
What to Do
- Use medicated shampoos 2–3 times a week to manage symptoms and prevent recurrence.
- During severe flare-ups, apply topical corticosteroids sparingly, following your healthcare provider’s instructions.
How Often
- Medicated shampoos: Use 2–3 times per week until symptoms improve.
- Corticosteroids: Apply once or twice daily for short periods, typically 1–2 weeks, to avoid side effects like thinning skin.
Additional Tips
- Avoid harsh shampoos or styling products that can irritate sensitive scalps.
- Follow a consistent treatment routine, as seborrheic dermatitis often requires long-term management (7).
4. Scalp Psoriasis
Psoriasis is an autoimmune condition that can affect the scalp, leading to thick, silvery plaques and localized hair loss. Though psoriasis does not directly damage hair follicles, scratching or aggressive treatments can weaken hair and increase shedding. Managing psoriasis effectively can minimize its impact on hair health (2).

Image: clevelandclinic.org
What You Need
- Topical treatments: Coal tar, salicylic acid, and corticosteroid-based products are effective for reducing plaques and inflammation.
- Phototherapy: UVB phototherapy can improve severe or treatment-resistant cases.
- Biologic therapies: Injectable medications like adalimumab or secukinumab target the immune pathways involved in psoriasis.
What to Do
- Apply topical treatments as directed, focusing on areas with plaques.
- For moderate to severe cases, consult a dermatologist about systemic therapies or phototherapy options.
How Often
- Topical treatments: Daily or as prescribed, typically for several weeks.
- Phototherapy: 2–3 sessions per week until symptoms are controlled.
Additional Tips
- Use a soft-bristled brush or comb to remove loose scales without irritating the scalp.
- Avoid excessive heat styling, as it can aggravate psoriasis symptoms.
5. Lichen Planopilaris (LPP)
Lichen planopilaris (LPP) is a rare inflammatory condition that affects the scalp and hair follicles. It is a type of scarring alopecia where inflammation damages the hair follicles, leading to permanent hair loss if untreated. Symptoms include redness, itching, scaling, and follicular plugging in the affected areas. Although the exact cause is unknown, LPP is believed to involve an autoimmune reaction. (2,7)

Image: remotederm.ca
What You Need
- Topical corticosteroids: Reduce inflammation in early stages.
- Oral immunosuppressants: Hydroxychloroquine, methotrexate, or corticosteroids for severe cases.
- Anti-inflammatory shampoos: Containing ingredients like salicylic acid or zinc pyrithione to soothe the scalp.
What to Do
- Apply corticosteroid creams or gels to the affected areas under medical supervision.
- For advanced cases, consult a dermatologist for systemic therapies that suppress immune overactivity.
How Often
- Topical treatments: Apply daily or as prescribed for several weeks.
- Oral treatments: Take as directed, typically over months, with regular monitoring by a healthcare provider.
Additional Tips
- Early intervention is key to preventing permanent hair loss. Seek professional help if symptoms like scalp redness or patchy hair loss appear.
6. Alopecia Areata
Alopecia areata is an autoimmune disease where the immune system attacks hair follicles, causing patchy hair loss on the scalp and other areas of the body. In some cases, it may extend to total scalp hair loss (alopecia totalis) or complete body hair loss (alopecia universalis). Though the condition itself does not cause scalp infections, secondary infections can occur due to frequent scratching or irritation of the scalp. (2.6.7)

Image: yalemedicine.org
What You Need
- Corticosteroids: Topical, injectable, or oral corticosteroids to suppress the immune response.
- Minoxidil: A topical solution that promotes regrowth in some cases.
- JAK inhibitors: Tofacitinib and ruxolitinib, newer therapies that target immune pathways involved in the condition.
What to Do
- Use topical corticosteroids or undergo corticosteroid injections directly into the affected areas to reduce inflammation.
- Apply minoxidil solution as prescribed to encourage hair regrowth.
How Often
- Corticosteroid injections: Administered every 4–6 weeks by a healthcare provider.
- Minoxidil: Apply twice daily for several months to see results.
Additional Tips
- Manage stress and maintain a healthy lifestyle, as these factors can influence flare-ups of autoimmune conditions.
7. Impetigo
Impetigo is a highly infectious bacterial skin illness caused by Staphylococcus aureus or Streptococcus pyogenes. It typically affects youngsters but may sometimes occur in adults. When impetigo affects the scalp, it leads to crusty sores that can damage hair follicles and cause temporary hair loss. (8)

Image: medicalnewstoday.com
What You Need
- Topical antibiotics: Mupirocin or fusidic acid ointments for localized infections.
- Oral antibiotics: Cephalexin or dicloxacillin for widespread or severe infections.
- Antibacterial cleansers: Products containing chlorhexidine or benzoyl peroxide to reduce bacterial spread.
What to Do
- Apply topical antibiotics to the infected areas as prescribed by a healthcare provider.
- For severe cases, take oral antibiotics to treat the infection systemically.
How Often
- Topical antibiotics: Apply 2–3 times daily for 7–10 days.
- Oral antibiotics: Take daily for 7–14 days, as directed.
Additional Tips
- Keep the scalp clean and dry to prevent the infection from spreading.
- Avoid close contact with others during the contagious phase of the disease.
8. Folliculitis Keloidalis Nuchae (FKN)
Folliculitis keloidalis nuchae is a chronic inflammatory condition that primarily affects the nape of the neck. It begins with small, itchy bumps at the hairline that can progress into keloid-like scars. The condition is most common in individuals with curly hair, and if untreated, it can lead to scarring alopecia. (2.7)

Image: medicalnewstoday.com
What You Need
- Topical antibiotics: Clindamycin or erythromycin to reduce bacterial involvement.
- Topical corticosteroids: Help reduce inflammation and itching.
- Laser hair removal: A long-term option to prevent recurrent follicular damage.
What to Do
- Apply topical antibiotics and corticosteroids as directed by a dermatologist to manage symptoms and prevent progression.
- Consider laser hair removal or other physical treatments to reduce hair density in affected areas.
How Often
- Topical treatments: Apply twice daily for several weeks.
- Laser treatments: Performed in multiple sessions, typically spaced 4–6 weeks apart.
Additional Tips
- Avoid tight collars or helmets that may irritate the nape of the neck.
- Maintain a clean and dry scalp environment to minimize bacterial growth.
9. General Scalp Care for Infection Prevention
Preventing scalp infections requires consistent hygiene practices and avoiding habits that damage the scalp or hair follicles. A healthy scalp environment supports hair growth and minimizes the risk of infections.
What You Need
- Mild shampoos and conditioners: Free from sulfates, parabens, and harsh chemicals.
- Nutrient-rich diets: Foods rich in vitamins A, C, D, and E, as well as biotin and omega-3 fatty acids, support scalp health.
What to Do
- Wash your hair regularly with a gentle shampoo, especially after sweating heavily or exposure to dirt.
- Incorporate a balanced diet with plenty of fruits, vegetables, and lean protein to nourish hair follicles.
How Often
- Shampooing: 2–3 times per week or as needed based on your hair type and activity level.
- Dietary adjustments: Daily, as part of a long-term strategy for healthy hair and scalp.
Additional Tips
- Protect your scalp from the sun by wearing a hat or using hair products with UV protection.
- Avoid hairstyles that pull tightly on the hair, as they can weaken follicles and increase breakage.
Final Words
Scalp infections can cause hair loss, but most can be treated successfully with the right care. Early diagnosis and proper treatment, such as medications and medicated shampoos, are key to preventing lasting damage. Good scalp hygiene and avoiding irritants can also help keep your hair and scalp healthy. If you notice signs of infection or unusual hair loss, see a dermatologist for advice and treatment. Taking quick action can protect your scalp and promote healthy hair growth.
Key Takeaways
- Scalp infections caused by fungi, bacteria, or autoimmune conditions can lead to temporary or permanent hair loss if not treated promptly.
- Effective treatment depends on the type of infection, with options ranging from oral antifungals and antibiotics to medicated shampoos and corticosteroids.
- Maintaining good scalp hygiene and using the appropriate medicated products can help manage and prevent infections.
- Early diagnosis and consistent treatment are crucial for minimizing damage to hair follicles and promoting regrowth.
- Preventive measures like avoiding shared hair tools, managing stress, and maintaining a nutrient-rich diet support overall scalp health.
Frequently Asked Questions
1. Can scalp infections cause permanent hair loss?
Yes, some scalp infections, such as folliculitis decalvans or untreated tinea capitis, can cause permanent hair loss if they result in scarring of the hair follicles. .
2. How do I know if a scalp infection is causing my hair loss?
Signs include redness, itching, scaling, pustules, or patches of broken or thinning hair. A dermatologist can confirm the diagnosis through an exam or tests.
3. What is the best treatment for fungal scalp infections?
Oral antifungal medications, such as griseofulvin or terbinafine, are the most effective treatments. Medicated shampoos containing ketoconazole can also help reduce surface fungal load.
4. Are over-the-counter products effective for scalp infections?
OTC products, like medicated shampoos with zinc pyrithione or salicylic acid, can help manage mild symptoms but are often insufficient for severe infections requiring prescription treatments.
5. How long does it take to treat a scalp infection?
The duration depends on the type and severity of the infection. Fungal infections typically require 4–8 weeks of treatment, while bacterial infections may resolve within 2–4 weeks.
6. Can I prevent scalp infections that lead to hair loss?
Yes, maintaining good scalp hygiene, avoiding sharing hair tools, and treating underlying conditions like seborrheic dermatitis can reduce your risk of scalp infections.
7. Should I stop using hair products during a scalp infection?
It’s best to avoid harsh or fragranced products that could irritate the scalp further. Stick to gentle, medicated shampoos recommended by your healthcare provider.
References
- Al Aboud, Ahmad M., and Jonathan S. Crane. "Tinea capitis." (2019).
https://www.ncbi.nlm.nih.gov/books/NBK536909/
- Wolff, Hans, Tobias W. Fischer, and Ulrike Blume-Peytavi. "The diagnosis and treatment of hair and scalp diseases." Deutsches Ärzteblatt International 113.21 (2016): 377.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4908932/
- Sosa, E. E., Philip R. Cohen, and Jaime A. Tschen. "Cladosporium scalp infection." Skinmed 10.6 (2012): 393-394.
https://pubmed.ncbi.nlm.nih.gov/23346670/
- Hadayer, Noa, et al. "Pemphigus vulgaris with loss of hair on the scalp." International Journal of Trichology 5.3 (2013): 157-158.
https://pubmed.ncbi.nlm.nih.gov/24574698/
- Khandpur, Sujay, and Belum Sivanagi Reddy. "Itraconazole therapy for white piedra affecting scalp hair." Journal of the American Academy of Dermatology 47.3 (2002): 415-418.
https://pubmed.ncbi.nlm.nih.gov/12196752/
- Nestor, Mark S., et al. "Treatment options for androgenetic alopecia: Efficacy, side effects, compliance, financial considerations, and ethics." Journal of cosmetic dermatology 20.12 (2021): 3759-3781.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9298335/
- Xu, Liwen, Kevin X. Liu, and Maryanne M. Senna. "A practical approach to the diagnosis and management of hair loss in children and adolescents." Frontiers in medicine 4 (2017): 112.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5522886/
- Johnson, Melinda K. "Impetigo." Advanced emergency nursing journal 42.4 (2020): 262-269.
https://pubmed.ncbi.nlm.nih.gov/33105179/





